summary
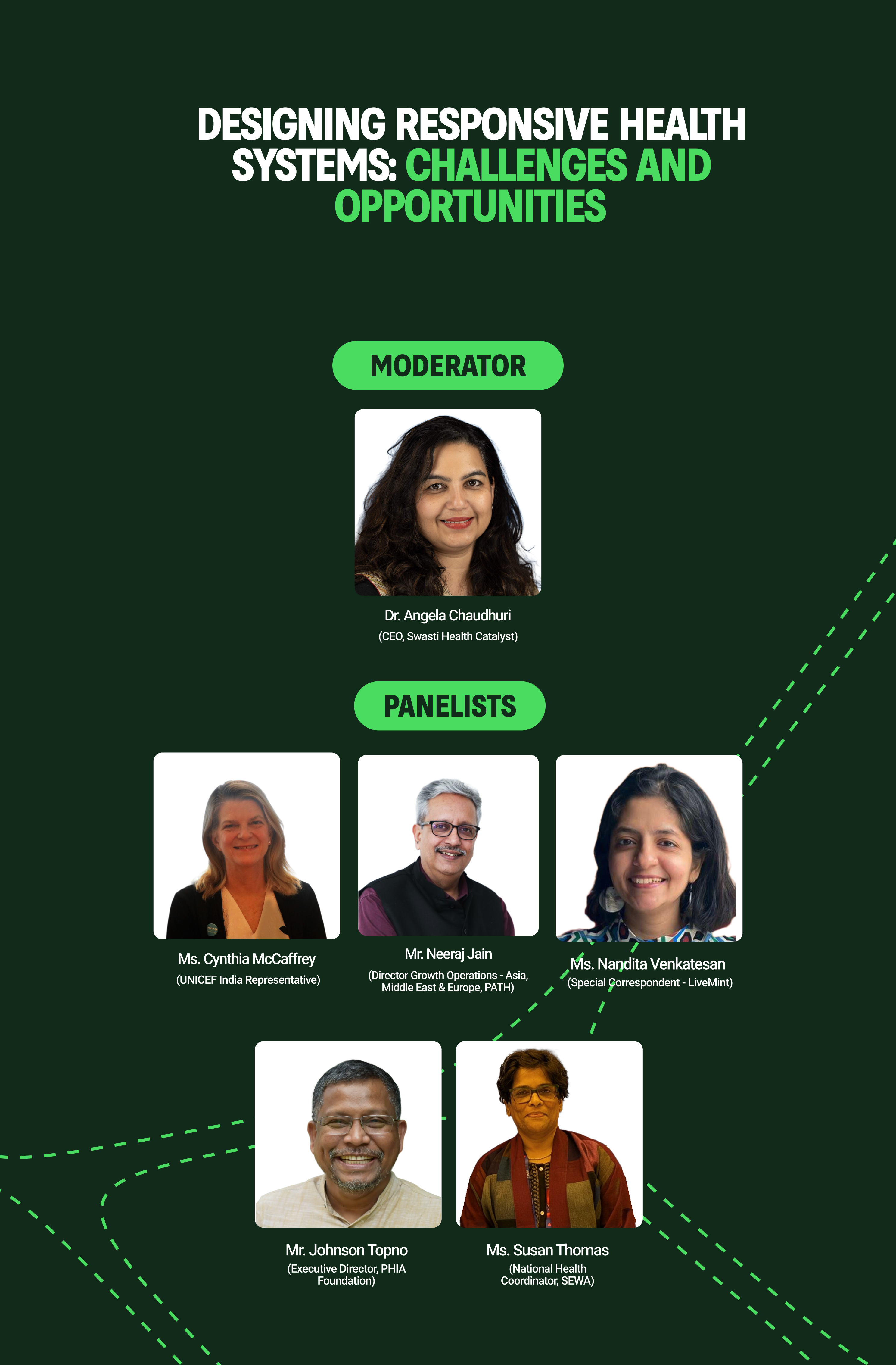
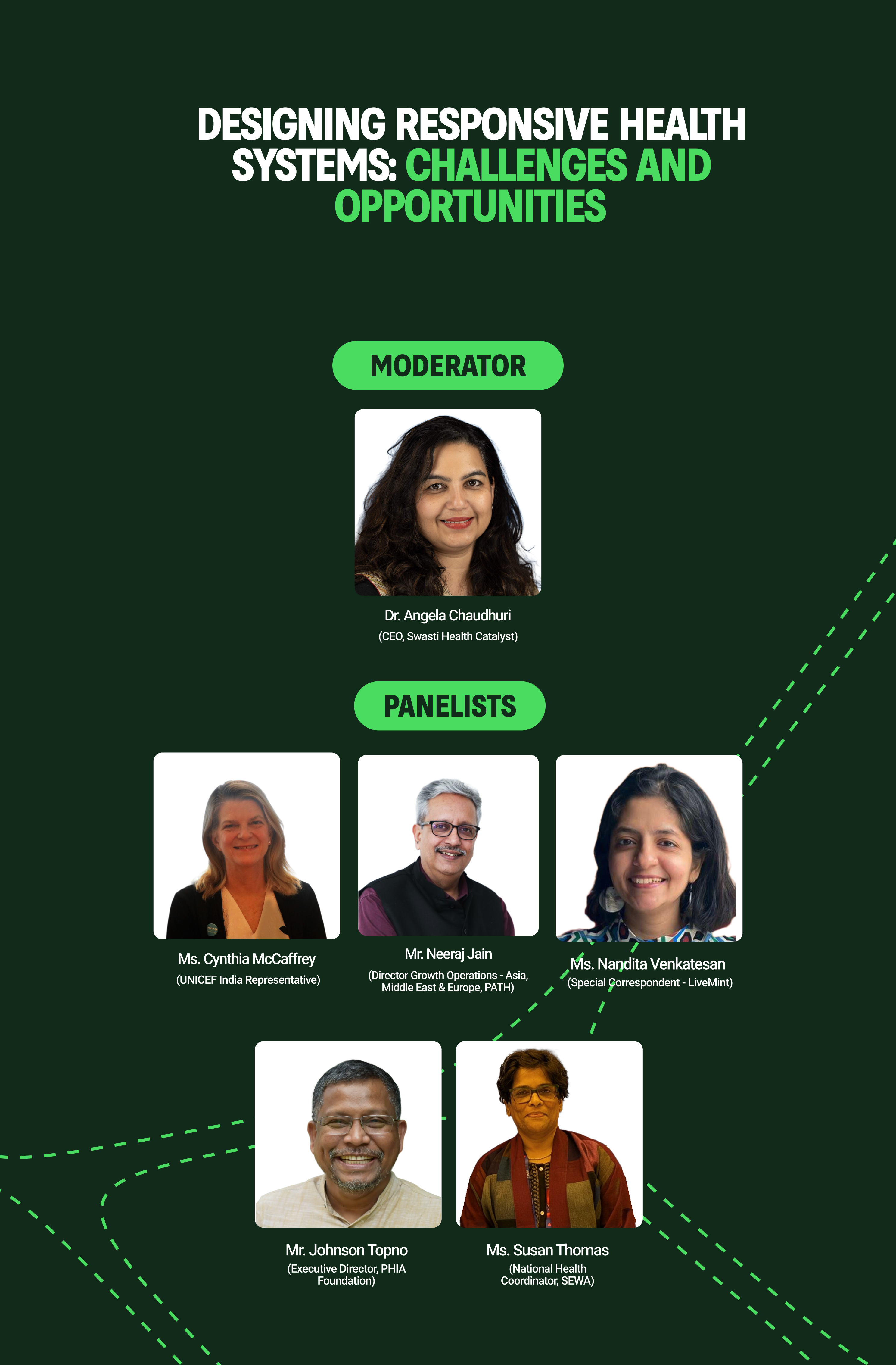
This panel underscored that health systems are not only about infrastructure or technology but about whether they are truly responsive to people’s needs. Cynthia McCaffrey (UNICEF India) opened by reminding us that India stands at a critical juncture on SDG 3: without inclusivity and urgency, the most vulnerable will continue to be left behind. Responsiveness, she argued, is about listening, adapting, and delivering in real time to the people who need care most.
Moderator Dr. Angela Chaudhuri highlighted a crucial paradox, that health systems often marginalize the very communities they are meant to serve. She framed responsiveness as a moral and practical obligation: unless systems amplify the voices of the unheard, they cannot be sustainable.
Panelists built on this theme from diverse vantage points. Susan Thomas (SEWA) illustrated how women in the informal sector continue to navigate health systems that ignore their lived realities, calling for greater focus on health literacy and self-advocacy. Johnson Topno (PHIA) spoke to the deep exclusion of tribal communities, emphasizing that participation through local institutions like gram sabhas is essential to shift the power dynamic in health decision-making.
Adding the perspective of lived experience, journalist and TB survivor Nandita Venkatesan noted how patients are often stigmatized as “non-compliant” when, in fact, they are making rational choices in systems that disregard their economic and social contexts. She reminded the audience that empathy is as critical as efficiency.
From the innovation and systems side, Neeraj Jain warned against “technology-first” solutions that look good on paper but fail frontline workers and patients. Instead, he called for living labs and co-designed models that begin with patients, not products. The panel converged on one central point: responsive health systems are not built by delivering to communities, but by creating with them.
Key takeaways
• Center communities in system design
Include affected populations from the start, ensuring solutions align with lived experiences rather than external assumptions.
• Invest in health literacy and agency
Especially for women and marginalized groups, enabling them to make informed choices and demand accountability.
• Adopt a “first mile” approach
Start with the most excluded and invisible communities instead of treating them as an afterthought.
• Strengthen local governance and accountability
Leverage community structures like gram sabhas to create mechanisms for responsive, bottom-up health systems.
• Embed empathy and trust in service delivery
Move beyond compliance-driven care to patient-partnered care that respects dignity.
• Back co-designed innovations
Support platforms that allow patients, providers, and innovators to design solutions together, not in silos.
• Redefine success and scale
Focus on depth of impact among vulnerable populations, not just headline numbers or tech adoption.
• Role for funders and platforms like BFI
Serve as conveners to bring lived experiences into decision-making and foster partnerships that bridge grassroots voices with scientific and technological innovation.
.png)
